Bone Marrow Transplants & Blood Transfusions – Why Is Blood No Longer an Option?
In Part 1, we compared the “Big 3” genetic test samples (Blood, Buccal, and DBS) and established that blood is the “Gold Standard.”
Today, however, we’re diving into the two critical situations where you must avoid using blood.
1. Case 1: Bone Marrow Transplant (BMT) Patients – “The Owner of the Blood Changes”
Let’s use an analogy. Think of your body’s bone marrow as a “blood factory.” This factory uses your personal DNA blueprint (your germline) to manufacture products like white blood cells and red blood cells.
✅ What is a Bone Marrow Transplant?
For treatment, chemotherapy and/or radiation are used to completely shut down the patient’s (Patient A’s) blood factory. Then, a healthy blood factory (hematopoietic stem cells) from a donor (Donor B) is transplanted into that empty space.
✅ Why is a Blood Test a 100% Error?
If the transplant is successful, Patient A’s body now has Donor B’s factory. This new factory produces blood using Donor B’s DNA blueprint.
- So, what happens if you draw Patient A’s blood for a test? -> You get 100% Donor B’s DNA.
- If a male patient (XY) receives a transplant from a female donor (XX)? -> That male patient’s blood karyotype test will come back as “Normal Female (XX).”
- The inherited genetic information for Patient A that we were looking for is not present in that blood. Not even 1% of it.
This state, where one body contains the genetic information of two different people, is called “Chimerism.”
✅ What’s the Alternative? -> ‘Buccal (Cheek) Swab’
“So, can these patients never get genetic testing?” Yes, they can. A buccal swab works perfectly. But why?
- Different Origins: The “blood factory” and the “cheek lining factory” (epithelium) come from completely different stem cell lines during embryonic development (Mesoderm vs. Ectoderm).
- Not Affected by the Transplant: A BMT is a procedure that only replaces the blood factory. It doesn’t touch the cheek factory.
- The Result: The cheek cells, regardless of the transplant, still contain 100% of Patient A’s original DNA.
1. BMT Patient’s Blood = Donor B’s DNA
2. BMT Patient’s Cheek = Patient A’s DNA
Therefore, a Germline test for a BMT patient must be done using a buccal (cheek) swab.
2. Case 2: Recent Blood Transfusion Patients – “The Blood is Temporarily Contaminated”
A transfusion is different from a transplant. You’re not swapping the factory, you’re just borrowing some finished products (blood) that you’re running low on.
✅ Why Won’t a Blood Test Work?
Even a standard bag of blood (like packed red blood cells) contains small amounts of the donor’s white blood cells (which contain DNA). When Patient A receives a transfusion, their bloodstream becomes a mix of DNA from multiple donors (Donor B, C, D…).
- The Result: [Patient A DNA] + [Donor B DNA] + [Donor C DNA]…
- When this “contaminated” sample is tested, the machine reads a jumble of mixed signals. This can lead to false negatives (missing the patient’s real mutation) or false positives (detecting a mutation that only the donor had).
✅ Is it okay if I only received Red Blood Cells (RBCs) and Platelets?
Theoretically, this makes sense, as RBCs and platelets have no genomic DNA (gDNA). However, in practice, the answer is still no.
- “Leukoreduction” (removing white blood cells) only reduces the WBC count to a standard-low level; it does not make it Zero.
- Zero is Technically Impossible: A small number of donor white blood cells always remain. Furthermore, modern tests like NGS involve an amplification process and are extremely sensitive. They can easily detect this low-level chimerism.
- Conclusion: As a best practice, if a patient has had any type of transfusion, it’s safest to wait the full 4 weeks.
✅ Why is it okay after 4 weeks? -> “The Immune System’s Big Cleanup”
Thankfully, this contamination isn’t permanent. The reason 4 weeks is the magic number is that it’s how long it takes for your body’s immune system to “clean house.”
- Recognized as an Invader: Patient A’s immune system identifies the donor’s white blood cells (from B, C, D…) as “non-self” (foreign invaders) and immediately begins to attack and destroy them.
- Short Lifespan: Even if some donor cells evade the initial attack, white blood cells themselves have very short lifespans (from days to a few weeks) and die off naturally.
“If 4 weeks is absolutely impossible, what’s the minimum time?” -> 2 weeks is the absolute minimum.
The 4-week (1-month) period is a “Safety Buffer” that ensures all of those “guest DNAs” have been completely cleared out by the patient’s immune system, leaving behind 100% the patient’s own blood.
Summary
Before any genetic test, it is critical to inform the medical staff of these two conditions.
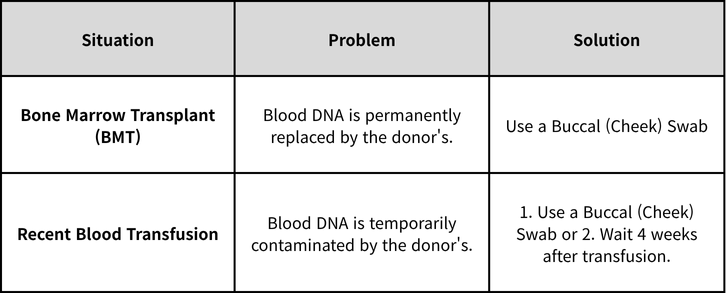
Knowing the patient’s precise medical history is the first and most important step to an accurate genetic test.
Explore the Full Sample Tips Series!
1️⃣ A Complete Guide to Genetic Testing Samples – Blood vs. Buccal vs. DBS
2️⃣ Bone Marrow Transplants & Blood Transfusions – Why Is Blood No Longer an Option?
3️⃣ The Buccal Swab Trap – “I Swabbed Your Cheek, So Why Is Their DNA Here?”
Get exclusive rare disease updates
from 3billion.

Sookjin Lee
Expert in integrating cutting-edge genomic healthcare technologies with market needs. With 15+ years of experience, driving impactful changes in global healthcare.