A Complete Guide to Genetic Testing Samples – Blood vs. Buccal vs. DBS
When testing for ‘innate’ Germline variations, every cell in our body shares the same DNA. “Theoretically,” a single strand of hair or a drop of saliva should be enough.
However, the preferred sample type clearly depends on two factors: “What kind of test is it?” and “What is the patient’s condition?”
Let’s break down the features and crucial considerations for the “Big 3” samples in genetic testing: Blood, Buccal (Cheek) Swabs, and Dried Blood Spots (DBS).
1. The Gold Standard: Blood
This is the most traditional and reliable method.
[Features]
- A 2-5mL venous blood draw. It is essential to use an EDTA (purple top) tube.
[Pros]
- Superior DNA Quality & Yield: Provides the highest concentration and purity of DNA.
- Highest Reliability: It is the “standard” sample type, best suited for high-throughput, precision analyses like WGS and WES.
[Cons]
- Requires Professional Staff: Must be drawn by trained medical personnel in a clinical setting.
- Invasive (It hurts): The use of a needle can cause pain and anxiety (needle phobia).
- Transport/Storage: Must use an EDTA tube. Requires refrigerated or frozen transport (a “cold chain”) depending on the season.
[Recommended For]
- Adult and pediatric patients requiring a definitive, high-quality diagnosis.
- Any case requiring high-throughput sequencing (WGS/WES).
2. The Easy & Painless Option: Buccal Swab
This is the fastest and least painful method for DNA collection.
[Features]
- A sterile swab or brush is used to scrape the inside of the cheek (buccal mucosa) 10-20 times.
[Pros]
- Non-invasive (Painless): Virtually no pain.
- Ease of Collection: Self-collection is possible (though ideally supervised within the clinic) if guidelines are followed.
- Simple Storage: Can be stored and shipped at room temperature using a preservation kit.
[Cons]
- Variable DNA Yield: The amount of DNA extracted can be insufficient, depending on the collection technique.
- Risk of Contamination: DNA from oral bacteria can be mixed in, reducing purity. (This leads to a slightly higher test failure rate than blood).
[Recommended For]
- Newborns and infants for whom a blood draw is extremely difficult.
- Adults with severe needle phobia.
- Situations requiring immediate sample collection within the clinic.
3. The Newborn Essential: Dried Blood Spot (DBS)
This is the standard screening method for (almost) every baby right after birth.
[Features]
- A few drops of blood from a small heel or finger prick are blotted onto a special filter card and allowed to dry.
[Pros]
- Minimally Invasive: Much less painful than a full venous draw.
- The Ultimate in Storage/Transport: Can be stored on the card for decades at room temperature, making transport incredibly easy.
- Standardized: It is the global standard for newborn screening programs.
[Cons]
- Low DNA Yield: For WGS/WES, at least 5 full, saturated spots are typically required.
- Extraction Difficulty: An extra step is needed to extract the DNA from the filter paper.
[Recommended For]
- All newborns (for national screening programs).
- Retrospective studies using banked, historical samples.
🚨 CRITICAL WARNING! Blood is NOT an option in these cases
We said blood is the “Gold Standard,” but there are two critical situations where blood must never be used for Germline testing. Ignoring this will lead to a 100% erroneous result.
1. Bone Marrow Transplant (BMT) Patients
- Why? A BMT replaces the patient’s entire “blood factory” (bone marrow) with a donor’s. The patient’s blood no longer contains the patient’s DNA; it is 100% the donor’s DNA. (This is called “Chimerism”).
- The Result: You end up testing the (likely healthy) donor’s genetics, not the patient’s inherited condition.
- Correct Sample: Buccal Swab. (Cheek cells are not affected by the transplant and still contain the patient’s original DNA).
2. Recent Blood Transfusion Patients
- Why? Transfused blood contains white blood cells (and thus, DNA) from the donor(s). The patient’s blood is temporarily contaminated with a mix of [Patient DNA + Donor DNA].
- The Result: The mixed DNA makes accurate analysis impossible. It can cause false negatives (missing a real mutation) or false positives (detecting a donor’s mutation).
- Correct Sample (Choose one):
1. Use a Buccal Swab.
2. If blood must be used, wait at least 4 weeks (1 month) after the last transfusion. (This is the time it takes for the patient’s immune system to “clean out” all the donor cells).
Summary
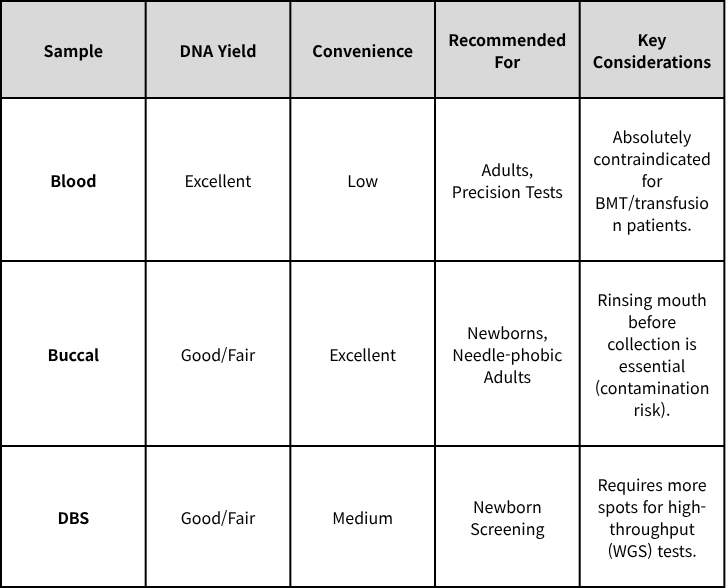
Conclusion: There is no single “best” sample. There is only the “optimal” sample that fits the patient’s condition and the test’s objective.
Coming up in Part 2: We’ll dive deeper into the “Chimerism” related to BMT and the fascinating topic of HLA matching that decides who can be a donor.
Explore the Full Sample Tips Series!
1️⃣ A Complete Guide to Genetic Testing Samples – Blood vs. Buccal vs. DBS
2️⃣ Bone Marrow Transplants & Blood Transfusions – Why Is Blood No Longer an Option?
3️⃣ The Buccal Swab Trap – “I Swabbed Your Cheek, So Why Is Their DNA Here?”
Get exclusive rare disease updates
from 3billion.

Sookjin Lee
Expert in integrating cutting-edge genomic healthcare technologies with market needs. With 15+ years of experience, driving impactful changes in global healthcare.