X-linked Agammaglobulinemia: diagnosis story
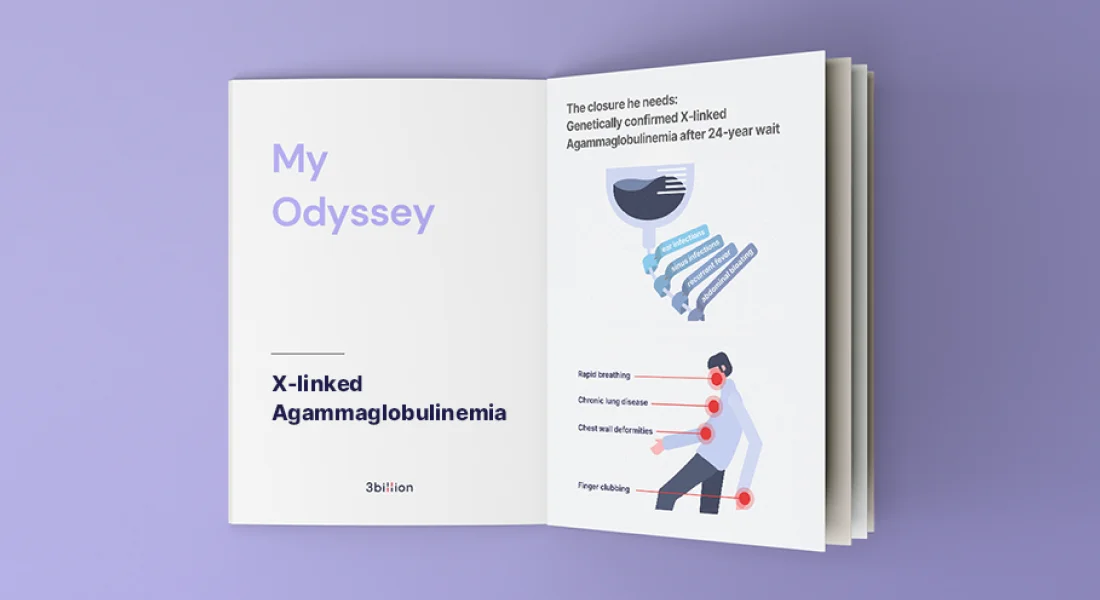
The closure he needs: Genetically confirmed X-linked Agammaglobulinemia after 24-year wait
We first saw Saravanan in our immunology clinic in 2021. Saravanan is a 40-year-old Indian man who was referred to us to establish a proper diagnosis for his underlying illness. He was initially managed by different doctors and later ended up without appropriate continuation of care in view of unavailability of immunologists in public hospitals in Malaysia. Fortunately, he was able to reach our team via the assistance of MyPOPI (Malaysian Patient Organisation for Primary Immunodeficiencies).
The Start of Saravanan’s Odyssey
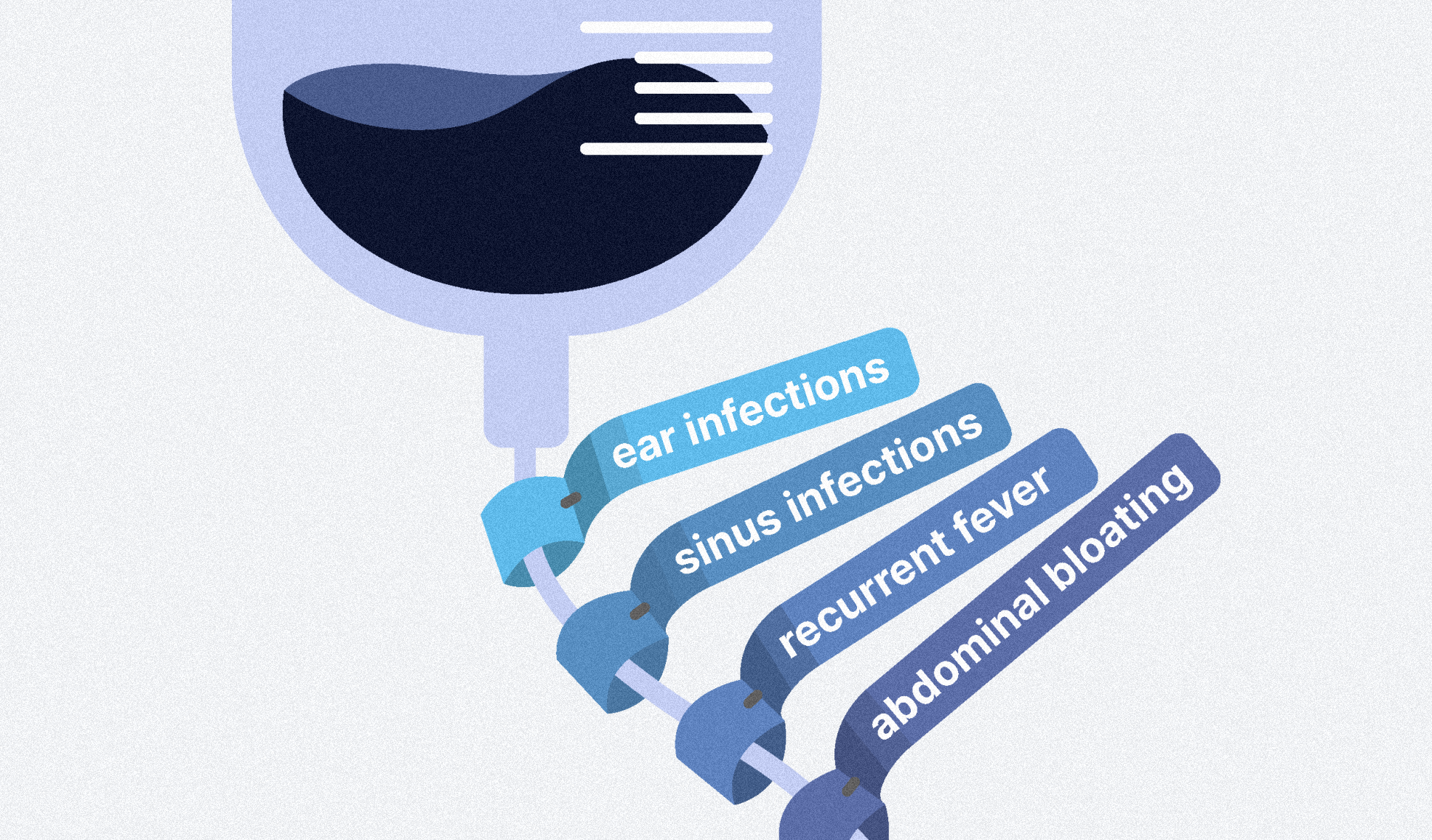
Saravanan was born to an Indian couple with no history of consanguinity. As far as he can remember, he was a healthy happy child until the age of 2 years. It was then that marked a life changing event whereby his left eye had to be enucleated due to severe infection. Following the devastating event, he had frequent episodes of ear infections, sinus infections, recurrent fever, and abdominal bloating which required multiple clinic visits, and luckily were resolved with symptomatic treatment. There was no similar history among his family members.
24 Years of Progressive Symptoms, Surgury, and Treatments
It was in the year 1997 when he was 16 years old, he had an episode of severe lung infection that had him admitted for 20 days. Initial blood tests showed he had low antibodies. Unfortunately, no further investigations were performed, and he was not properly followed up. He was started on antibody treatment at only the age of 17 years. This treatment known as intravenous immunoglobulin (IVIG), was given at a frequency of 4 times a week for one year, but was forced to stop due to financial difficulties.
He was struggling due to his low income which was not enough to bear the huge cost of IVIG. At the age of 24, the IVIG was restarted at 4 to 6 week intervals intermittently with no regular follow-up. During this period, his lung function worsened as a result of bronchiectasis, in which his airway walls became irreversibly thickened, damaged, and scarred. He also had arthritis of both small and large joints and recurrent abdominal pain with diarrhea needing anti-diarrhea (loperamide three times/week).
To make matters worse, he started to have palpitations with difficulty to breath around the young age of 31 years old. He was referred to the National Heart Centre and was diagnosed with chronic rheumatic heart disease. A year after diagnosis, he had to undergo heart surgery to replace one of his damaged heart valves. Due to the valve replacement, he is on lifelong blood thinner treatment (known as an anticoagulant) to prevent blood clots and reduce the risk of heart attacks and stroke.
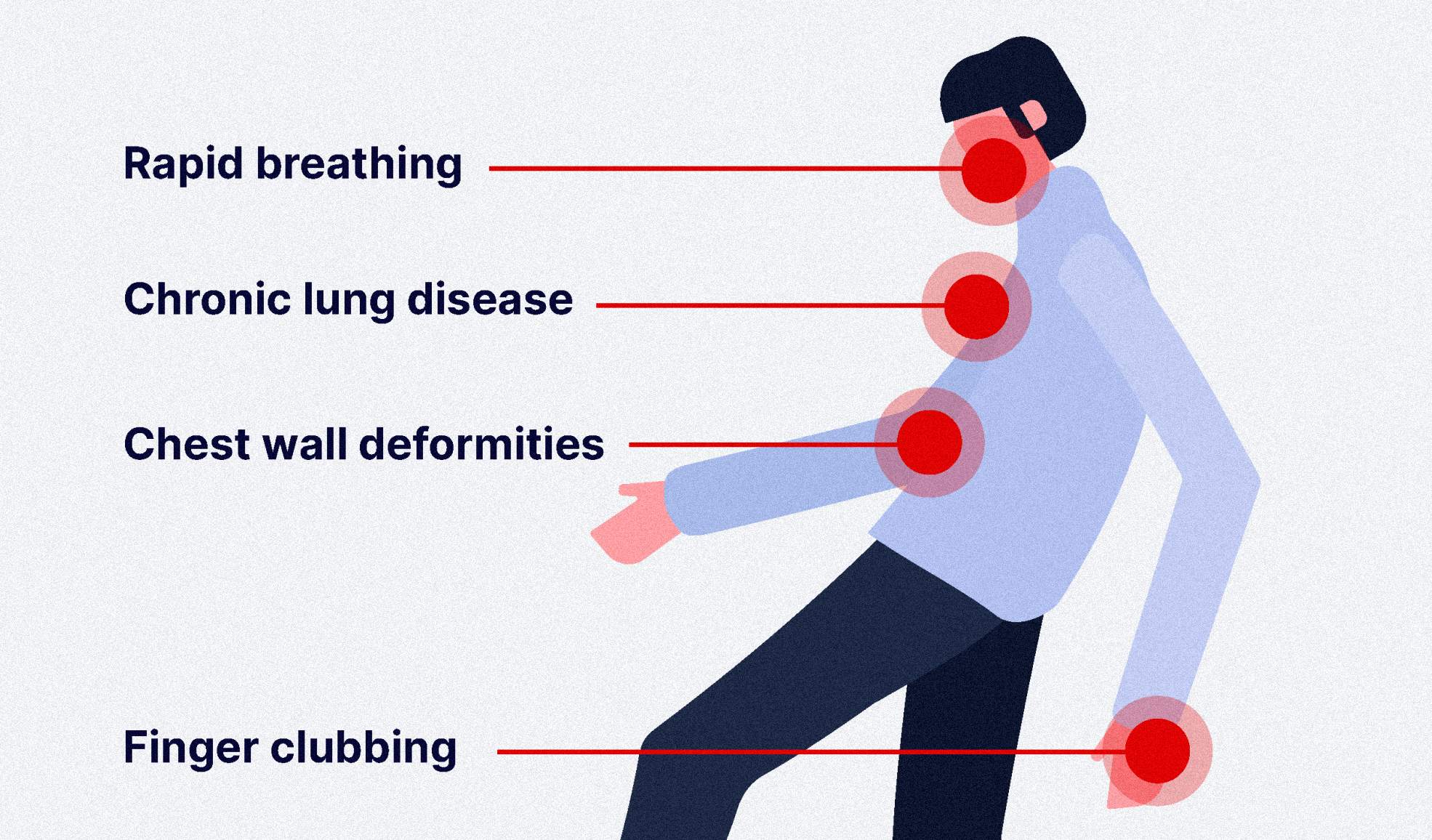
Upon clinical examination, Saravanan was a thin man with slight, rapid breathing. There were signs of chronic lung disease indicated by grade 4 finger clubbing and chest wall deformities. He had absent tonsils, a mildly enlarged liver, and an audible click on heart examination. Investigations done in our center revealed absent B cells and low levels of antibodies (IgA, IgM and IgE). Antibody IgG was highly probable because he had just received IVIG treatment a few days prior.
We managed to send his blood samples to 3billion’s laboratory in South Korea since we had a collaborative project with the company. After a long 24 years of waiting, the definitive diagnosis of X-linked agammaglobulinaemia (XLA) was established via genetic testing whereby a mutation in the BTK gene was found.

We have optimised his IVIG dose and frequency to 4-weekly intervals, and referred him to the gastroenterology team for the inflammatory bowel disease work-up and rheumatology team for the arthritis work-up.
Professor Dr. Intan Hakimah’s biography
 |
Associate Professor Dr. Intan Hakimah Ismail is currently the Head of Clinical Immunology Unit at the Faculty of Medicine and Health Sciences, Universiti Putra Malaysia (UPM) and Senior Consultant Pediatrician and Consultant Clinical Immunologist & Allergist at the Hospital Pengajar UPM (HPUPM). She obtained her subspecialty and PhD in Allergy and Clinical Immunology from the University of Melbourne, and Murdoch Children’s Research Institute, Melbourne, Australia. The current major focus of her research team is on exploring the genetics of primary immunodeficiency diseases (PID). Her goal is for more PID patients to have widespread access to genetic testing in Malaysia. With genetic testing, PID patients will receive accurate and timely diagnoses, which is crucial for successful and better treatments; a step towards personalized medicine.
Get exclusive rare disease updates
from 3billion.

Sree Ramya Gunukula
Marketing Leader with experience in the pharma and healthcare sectors, specializing in digital health, genetic testing, and rare disease diagnostics.