Chromosomal Microarray Test: What Does a Negative or Normal Result Mean?
If you or your loved one has undergone a Chromosomal Microarray Analysis (CMA), you might be feeling a mix of emotions – anticipation, concern, or even curiosity about what the results might reveal. It’s a journey that many embark on with hopes of gaining insights into genetic health. In the following article, we delve into the world of CMA, aiming to provide clarity and understanding to those awaiting or interpreting their results, especially when they are negative or normal.
Chromosomal Microarray (CMA)
CMA, also known as array comparative genomic hybridization (array CGH) or SNP microarray, has revolutionized genetic diagnostics. It is instrumental in identifying chromosomal variations, such as deletions or duplications, which are key in diagnosing genetic diseases.
What is Chromosomal Microarray?
Chromosomal Microarray Analysis (CMA) is a sophisticated and comprehensive genetic test that plays a crucial role in modern medical diagnostics, particularly in the realm of genetics. Understanding what CMA is and how it works is vital for anyone navigating the complexities of genetic health.
CMA is an advanced tool used to detect chromosomal abnormalities at a level of detail that was previously unachievable with traditional genetic testing methods. It scans the entire genome, which is the complete set of your DNA, including all of your genes. This thorough examination allows for the detection of even the smallest changes in chromosomes, known as microdeletions and microduplications.
Unlike conventional karyotyping, which can only detect large chromosomal abnormalities, CMA can identify much smaller changes that are often the culprits behind various genetic disorders. It examines the genome for missing (deletions) or extra (duplications) pieces of DNA, providing insights into genetic anomalies that could be responsible for certain medical conditions or developmental delays.
Understanding CMA Test Procedures
CMA testing involves comparing a patient’s DNA with a control to identify chromosomal imbalances.
How is CMA Testing Conducted?
Chromosomal Microarray Analysis (CMA) testing is a sophisticated process that involves several steps, from sample collection to data analysis. Understanding how CMA testing is conducted can provide clarity and alleviate concerns for those undergoing or considering this test.
Sample Collection
The first step in CMA testing is the collection of a DNA sample. This is typically done through a blood draw, which is a standard and straightforward procedure. In some cases, other types of samples, such as saliva or skin tissue, can be used. The choice of sample type can depend on the patient’s condition, age, and other factors.
DNA Extraction
Once the sample is collected, the next step is extracting DNA from it. This involves breaking down the cells in the sample to release the DNA. The DNA is then purified to ensure that the sample is clean and suitable for analysis.

Preparing the DNA for Analysis
The extracted DNA is then processed and labeled with a special dye. This labeling allows the DNA to be visualized and analyzed during the CMA process. The patient’s DNA is usually labeled with one color, while a reference DNA sample (used for comparison) is labeled with a different color.
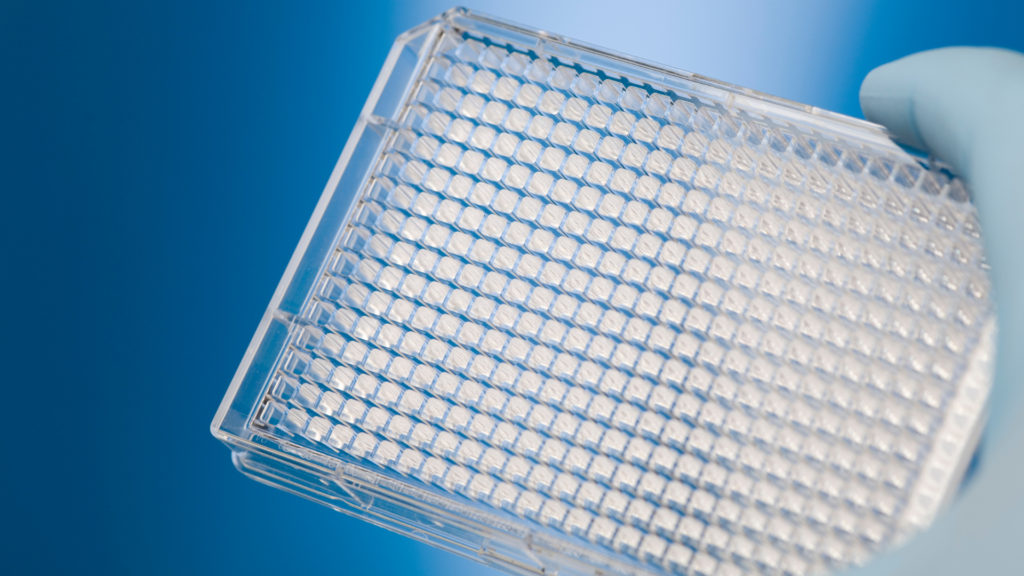
Hybridization
The CMA process involves hybridization, where the patient’s DNA is applied to a microarray chip. This chip contains thousands of tiny DNA probes, each corresponding to a specific region of the human genome. The patient’s DNA binds, or hybridizes, to these probes. Simultaneously, the reference DNA sample is also hybridized to a separate array.
Scanning and Analysis
After hybridization, the microarray chips are scanned using specialized equipment. This scanner detects the fluorescent signals from the labeled DNA, which indicate where the patient’s DNA has bound to the probes. The intensity of these signals is then analyzed to identify any imbalances in the DNA.
Interpreting the Data
The data from the scan are interpreted by geneticists or specialized laboratory professionals. They compare the patient’s DNA to the reference DNA, looking for differences in the intensity of the signals. These differences can indicate the presence of extra or missing segments of DNA in the patient’s genome.
- Deletions: If a segment of DNA is missing in the patient’s sample, the corresponding area on the microarray will show a weaker signal compared to the reference.
- Duplications: Conversely, if there is an extra segment of DNA, the signal will be stronger.
Reporting the Results
The final step is compiling the findings into a report. This report details any genetic abnormalities found and their potential significance. It’s important to note that the interpretation of CMA results can be complex, and they are typically discussed with the patient by a genetic counselor or a healthcare provider. This discussion helps in understanding the implications of the results for the patient’s health and potential future medical decisions.
How Long Does Chromosomal Microarray Test Results Take?
The duration to receive chromosomal microarray test results can vary based on the laboratory and the complexity of the case. Typically, results are available within 2 to 4 weeks. However, certain factors, such as the need for additional analysis or re-testing, can extend this timeframe. Always check with your healthcare provider or testing facility for more specific details regarding result turnaround times.
How much does a chromosomal microarray test cost?
The cost of a chromosomal microarray test can vary depending on the laboratory and geographic location. Insurance coverage may also affect the out-of-pocket cost, with many insurance plans covering part or all of the test if it’s deemed medically necessary.
Types of Samples Used for CMA Testing
Chromosomal Microarray Analysis (CMA) testing requires a DNA sample, and the type of sample used can vary based on the specific circumstances of the patient and the purpose of the test. Understanding the different types of samples that can be used for CMA testing is important for patients and healthcare providers as they prepare for this genetic test.
Blood Samples
The most common type of sample used for CMA testing is blood. Blood samples are widely preferred because they are relatively easy to collect and typically provide a sufficient amount of high-quality DNA for the analysis. A standard blood draw is conducted, where a small amount of blood is taken from a vein, usually in the arm. This method is used for both children and adults.
Saliva Samples
In some cases, particularly when a blood draw is not feasible or is challenging (like in the case of infants or patients with certain medical conditions), saliva can be used as an alternative. Saliva samples are collected using a special kit where the individual is asked to spit into a tube or swab the inside of their cheek. While saliva samples are generally less invasive to collect, they might sometimes yield lower quantities of DNA compared to blood samples.
Tissue Samples
For certain conditions or in specific contexts, such as prenatal testing or post-mortem analysis, tissue samples might be used. This can include amniotic fluid, chorionic villus sampling (CVS), or even skin biopsies. These types of samples are more invasive to collect and are typically used when specific genetic information about the fetus or in specific medical cases is needed.
Amniotic Fluid and Chorionic Villus Sampling (CVS)
In prenatal CMA testing, amniotic fluid (collected through amniocentesis) or placental tissue (collected through CVS) can be used. These procedures are more invasive and carry some risks, so they are generally performed when there is a high risk or suspicion of genetic abnormalities in the fetus.
Chromosomal Structures and Their Significance in CMA
Chromosomes, made up of genes, are structures within cells that dictate bodily functions and traits. Each cell normally contains 46 chromosomes, arranged in 23 pairs. Chromosomal anomalies detected by CMA are crucial for diagnosing genetic diseases.

Wondering How Gene Panel Compares to Exome Sequencing?
Learn how WES provides greater diagnostic accuracy compared to gene panels
Interpreting CMA Results
CMA results vary, each with its own clinical significance.

Different Types of CMA Results
- Normal Results: Indicate no significant chromosomal imbalances. However, they do not confirm the absence of all genetic disorders.
- Likely Pathogenic Results: Suggest the potential presence of health issues due to chromosomal imbalances.
- Variants of Unknown Significance (VUS): Present uncertain findings, often necessitating further testing.
- Regions of Homozygosity (ROH): Indicate genetic similarities that could be clinically significant.
What does a negative or normal microarray mean?
Negative or normal CMA results mean no significant chromosomal abnormalities were detected. Nonetheless, they don’t conclusively rule out all genetic disorders. These results suggest that the tested chromosomal segments are free from deletions or duplications detectable by CMA. However, CMA has limitations, and many genetic conditions caused by minute DNA differences remain undetectable.
Additional Genetic Testing After Negative CMA Results
When Chromosomal Microarray Analysis (CMA) results come back negative or normal, indicating no significant chromosomal abnormalities, it might be the end of one path of investigation, but it can also be the beginning of another. In many cases, additional genetic testing is recommended after a negative CMA result, especially if the clinical symptoms or family history suggest a genetic condition. Understanding why further testing is necessary and what it entails can provide valuable guidance for patients and families navigating these complex scenarios.
Why Further Testing is Necessary
- Limitations of CMA: How accurate is chromosomal microarray analysis?While CMA is a powerful tool for detecting chromosomal deletions and duplications, it does not identify all types of genetic abnormalities. For instance, CMA cannot detect point mutations or smaller genetic changes that can be responsible for many genetic disorders.
- Unresolved Symptoms: If a patient continues to exhibit symptoms or clinical features suggestive of a genetic condition, despite a negative CMA result, further testing can be crucial in reaching a diagnosis.
- Advances in Genetic Testing: The field of genetics is rapidly evolving, with new tests and methodologies emerging that can provide deeper insights into complex genetic cases.
Types of Additional Genetic Tests and Their Importance
- Whole Exome Sequencing (WES): This test examines all the protein-coding regions of genes in the genome, known as the exome. It can detect single nucleotide changes or small insertions and deletions in these regions, which might be the cause of genetic disorders.
- Whole Genome Sequencing (WGS): WGS involves examining the entire genome. It is more comprehensive than WES and can detect a wide array of genetic changes, including those in non-coding regions of the DNA.
- Targeted Gene Panels: These are tests that look at a select group of genes known to be associated with specific conditions. They are particularly useful when a specific genetic disorder or a group of related disorders is suspected.
- Mitochondrial DNA Testing: This type of testing is used if a mitochondrial disorder is suspected. Mitochondrial DNA is separate from the DNA found in the cell nucleus and requires different testing methods.
If your Chromosomal Microarray Analysis (CMA) results have left you with concerns or questions, know that your feelings are completely valid and shared by many. Navigating the world of genetic testing can be a complex and emotional journey, one that often brings a mix of worry and hope.
It’s important to remember that these results, whether negative or normal, are not the final word on your health journey. They are, instead, a part of a larger, ongoing conversation about your genetic health. Further testing and consultations with healthcare professionals can provide more comprehensive insights, guiding you towards a clearer understanding of your genetic makeup.
About comprehensive diagnosis process
References
https://microarray.bsc.gwu.edu…
https://www.ncbi.nlm.nih.gov/p…
https://www.jax.org/education-…
Get exclusive rare disease updates
from 3billion.

Sree Ramya Gunukula
Marketing Leader with experience in the pharma and healthcare sectors, specializing in digital health, genetic testing, and rare disease diagnostics.